The AN-ACC NWAU has been announced. Here’s what to do now
March 30, 2022 | AN-ACC
By Tyler Fisher, Data Scientist
The Australian National Aged Care Classification (AN-ACC) is scheduled to be implemented on 1st October 2022 as part of the Aged Care reforms announced one year ago. At the same time, a 10% increase to subsidy expenditure was also announced. The AN-ACC mechanism will require the Government to make an annual determination about the funding (price) of a National Weighted Activity Unit (NWAU). This price is standard across both the fixed (same across facility) and variable (individual to each resident) components. All rates in the funding model are then set relative to this annually determined price. For those familiar with the national hospital funding model, this price is termed the National Efficient Price (NEP).
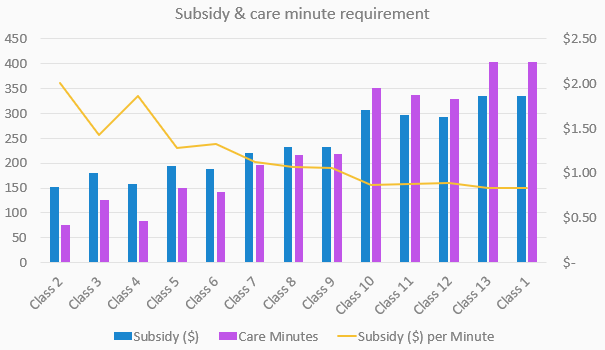
There is further additional funding budgeted as part of the broader reforms which is designed to offset an increase to frontline care staff in the lead up to a mandated care minute requirement. This is because the new funding model requires that each service will deliver a minimum care minute per resident linked to their AN-ACC classifications.
Average resident funding expected to be $225 per day
In the Budget announcements on 29 March 2022, the inaugural residential aged care AN-ACC NWAU starting price is $216.80. At this starting price, average resident AN-ACC funding is expected to be approximately $225 per day and with it, the financial impact to services has become more real. Along with the associated subsidy rates of each classification there is also increased visibility of the care minute requirement for each classification. This must be compared to current service rosters to understand the net financial impact at each facility.
This scatter plot diagram demonstrates the variable impact of AN-ACC on providers across the sector.
Click on image to expand
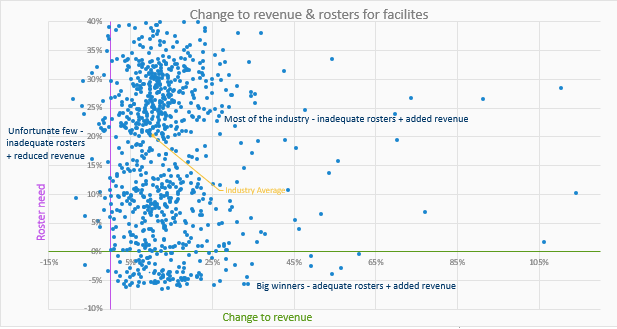
The two variables will be the relative performance of your ACFI to industry, and the relative amount of care time you are currently delivering. Most of the industry will fall around the average and have inadequate care time in their rosters but benefit from the added revenue of the new funding. The big winners will be those who are already outperforming the industry average for care minutes so will not need to adjust their costs but will benefit from the increase to their top line funding. An unfortunate few will see increases to their costs and potentially reduced revenue. These few will currently have high subsidy revenue due to practices that are supported by ACFI but not directly funded by the new AN-ACC mechanism.
Budgeting and resource planning
As at 9 March, more than 68% of residents have already undertaken an AN‑ACC assessment through the shadow assessment process and the Department is forecasting that all the providers in the industry will have had at least one facility reviewed by the end of March 2022. The release of the first results of those assessments could therefore follow soon after. This will be the other piece to the puzzle as the classification results with the AN-ACC NWAU price will give providers their first practical look at the financial outcomes of the new model.
Providers preparing budgets and resource plans are keen to receive this further information on the outcomes of the shadow assessments as soon as possible and many providers have been busy estimating the AN-ACC case mix of their resident populations.
This has three advantages.
- The first is that they are getting a head start learning a new model and implementing new strategies as quickly as possible. The training component for the new model will be significant and the early it is begun, the more manageable it will be.
- The second is that when the shadow assessment information is made available, they will have a data set to reconcile the shadow assessment results to and prepare for any reassessment claims.
- The third reason is that the industry will no longer be able to only consider the regular increase of Average Daily Subsidy (ADS) as a measure of good performance because each facility will have its own care time target based on the AN-ACC case mix of residents, so as subsidy increases so directly will the care time target and cost.
The need to have stability in costs, including the largest cost (clinical staff) combined with the need to provide staff with consistency in their rostered shifts means that case mix will need to be stabilised. Admissions decisions and reappraisal strategies designed to maximise subsidy might be reengineered to flatten ADS trend lines. Providers are now incentivised to reclassify residents to a lower classification when it is appropriate to do so. This is obviously a big departure from current ACFI strategy and means that the decisions of if and when to reclassify a resident become more complex.
Click on image to expand
Meeting, reporting and compliance for care minutes
From July 2022, reporting on care minutes will become quarterly and in December 2022 services and care minutes data reports will inform a Star Rating system which will allow senior Australians to compare staffing levels between facilities and help them make an informed choice about their care. From October 2023 providers will meet, and report on, a mandatory care time.
Further legislation will come to define the implications of failing to meet the mandate beyond the compliance to a star rating. Consistently meeting the mandate daily, while also retaining a sustainable operational result (subsidy less cost of care) will require modelling resident movements and reclassification decisions.
These changes will require a new level of focus on the analysis of this data and for some providers, new skillsets, or roles in the organisation. We are currently working with many organisations on these transitions so if you would like to learn more about the implications to your business or the broader reforms, please contact us.